INTRODUCTION
An anterior cruciate ligament (ACL) injury is the most common knee joint injury among over 250,000 physically active young individuals in the United States each year [1]. Individuals who suffered ACL rupture tend to choose either a non-surgical or a surgical intervention. The anterior cruciate ligament reconstruction (ACLR) surgery is intervened to restore the structural deficiencies. Even if structural stability is restored after ACLR, quadriceps muscle atrophy is seen in those who underwent ACLR [2]. Based on magnetic resonance image (MRI) and ultrasound, which are equipment for measuring the morphology of muscles, it was revealed that the muscle volume, cross-sectional area (CSA), and thickness were decreased [2–4]. Previous studies reported that individuals who underwent ACLR showed atrophy of the quadriceps muscle of the involved limb compared to the uninvolved limb[2,3,5]. Finally, quadriceps muscle atrophy increases the risk of knee osteoarthritis (KOA) and ultimately produces adverse effects such as lowering an individual’ s quality of life [6–8].
Despite completion of rehabilitative exercise or therapy to return to sports/daily life after ACLR, quadriceps muscle weakness resulting from muscle atrophy remains a concern [9,10]. In addition, quadriceps weakness can lead to an increased risk of ACL reinjury in the future. This quadriceps muscle strength is a modifiable factor during rehabilitation after ACLR [11]. Quadriceps function is important because it is associated with knee stability [12], functional performance [13], self-reported function [11], return to sports/daily[14], and risk of secondary ACL injuries [15]. The ACLR patients showed not only muscle atrophy, but also lower functional performance compared to unaffected side or healthy. The significance of muscle size is emphasized because such muscle size is closely related to functional performance [16].
The ACL reinjury rate after ACLR among young players is as high as about 30% [17]. As such, it is important to return in a timely manner to avoid the risk of secondary ACL injuries. Recently, objective “ criteria” for impairment and functional status have been proposed for successful return to sports/daily activities. It is generally known that the standard for return to sports athletes from ACLR is 6 months. However, previous studies showed that ACL reinjury was highest between 6 to 12 months after ACLR [15,18]. To prevent ACL reinjury after ACLR, a return to sport criterion of at least 9 months is recommended [15]. The criteria for deciding to return are often evaluated by hopping and strength tests [19]. These tests are usually performed between 6 to 12 months after ACLR [15,20]. Among the various hop tests, the single-leg hop test is the most common assessment method for evaluating functional performance [21]. The isokinetic strength test, which is commonly used as a strength test, is a useful method to evaluate the strength and function of bilateral knee strength and function [22]. A difference in bilateral quadriceps muscle strength of less than about 15% can be established as a proper criterion of return to sports [18]. If the difference in quadriceps muscle strength between the affected side and the unaffected side is large, the risk of secondary ACL injury or injury to the contralateral limb may increase [15]. For this reason, it is important to prevent muscle loss of the quadriceps muscle on the affected side after ACLR.
Although muscle hypertrophy and muscle atrophy can be indicated as objective indicators with the thickness of the muscle, a clear standard for return to sports/daily has not been established. Also, since the research results to determine the return to muscle size are insufficient, it is necessary to evaluate the size and function of the muscle according to the criteria. Therefore, the purpose of this study is to present an evi-dence-based recommendation for returning to sports from ACLR by evaluating muscle size and function based on less and more than 9 months after ACLR.
METHODS
1 Participants
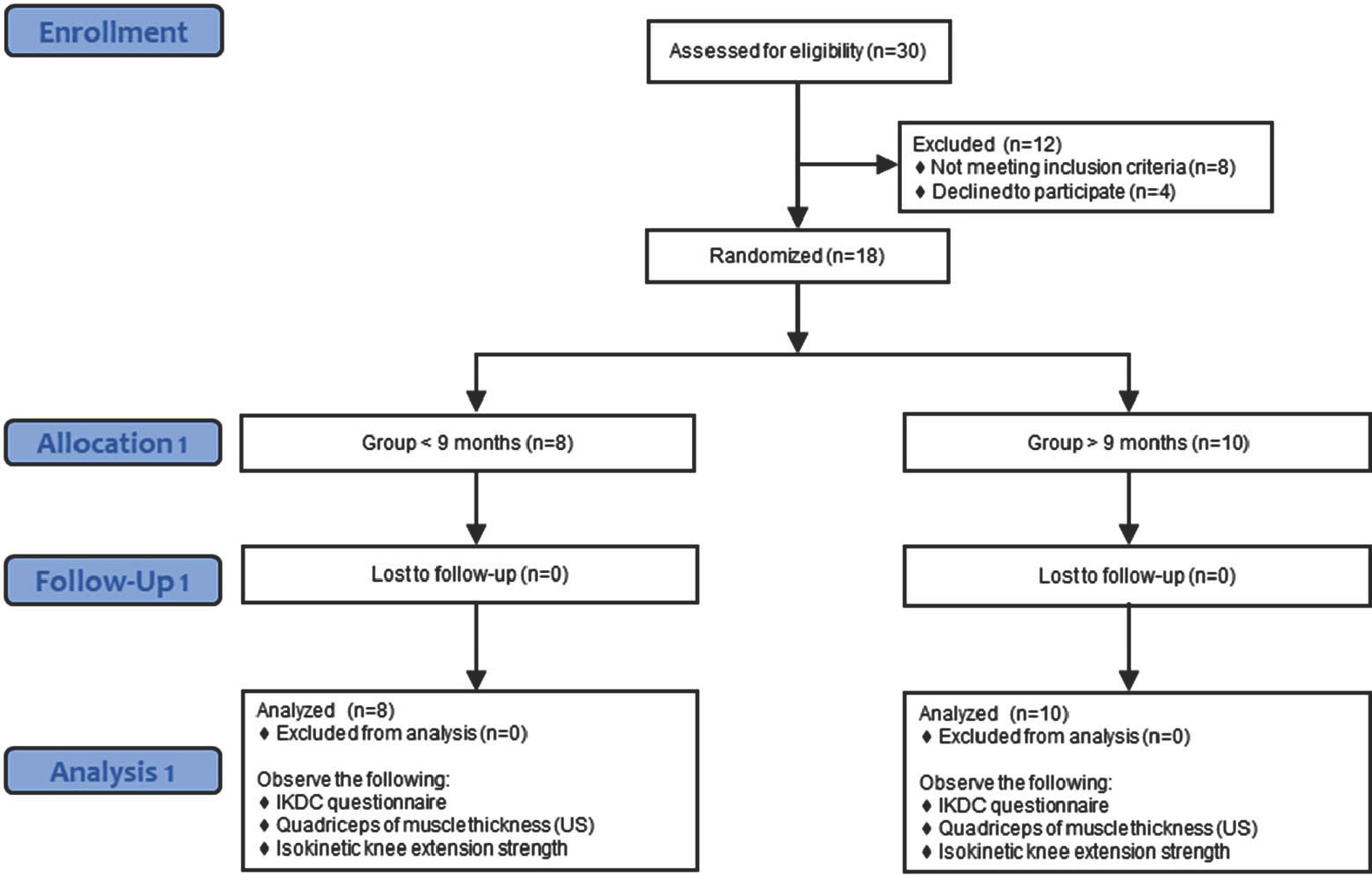
A total of 18 individuals who underwent ACLR voluntarily participated in this study (Table 1). Participants in the current study were divided into two groups based on 9 months after the ACL reconstruction. The participants in this study consisted of people with a history of ACLR due to a complete rupture. The following cases were excluded from this study: 1) Unable to be observed with an ultrasound device due to hema-toma or edema, 2) an acute injury in the lower extremity, 3) impossible to perform the functional tests due to pain in the lower extremity as well as knee joint, 4) a history of ACLR in both limbs, 5) meniscus or other ligaments injury with ACL injury.
2 Research procedures
The flowchart of the current study is presented in Fig. 1.
This study was approved by the Inha university’ s Institutional Review Board (Study ID: 190404). All participants signed a consent form to participate in this study after completely understanding the contents of this study. They wore comfortable clothes to participate in this study and completed a self-reported questionnaire before measuring muscle thickness and isokinetic knee extension strength. Participants performed the test barefoot to measure the variables. Muscle thickness was first measured to obtain images of relaxed muscles before measuring isokinetic knee extension strength. After measuring the muscle thickness of the participant’ s bilateral quadriceps, the isokinetic knee extension strength was measured. The isokinetic knee extension strength test was performed after the participants warmed up for 5-minute on a cycle ergom-eter at 40-50 rpm [23].
3 Self-reported questionnaires
Participants evaluated knee conditions through self-reported questionnaires before measuring functional performance and muscle thickness. The International Knee Documentation Committee (IKDC) questionnaire consists of 18 questions in three categories: knee symptoms, function, and sports activity [24]. To calculate the questionnaire score, the sum of the scores for each item minus the lowest score is divided by the highest possible score, then multiplied by 100 [24]. The score is expressed on a scale from 0 to 100, and a higher score means better knee function [24]. IKDC shows a high test-retest reliability (0.94) and a high coefficient alpha value (0.92) [24]. It was expressed as a percentage ranging from 0 to 100.
4 Measurement of muscle thickness
To measure the quadriceps muscle thickness, it was used the portable wireless ultrasound device (SONON 300L, Healcerion, Korea). The ultrasound equipment was set to B-mode (Gain: 53%, DR: 54dB, TGC: 48%, Filter – Frame average: 3, SRI: 4, Gray map: F). Each participant was assessed in a relaxed supine position with both knees extended and toes pointed to the ceiling to prevent the hip external rotation. The measurement of ultrasound device was performed by an expert who was fa-miliar with the equipment to avoid inter-individual variability. Before measuring the thickness of each muscle, the participant’ s hair was shaved and the skin cleaned to obtain an accurate image. The transducer was placed perpendicularly with minimal pressure on the long axis of the thigh. To measure the RF and VI muscle thickness, a transducer was placed at 50% of the distance between the anterior superior iliac spine (ASIS) and superior pole at the patella. The RF muscle thickness was defined as the distance between the superficial border and deep border of the muscle. The VI muscle was located below the RF, which is defined as the distance between the superficial border of the muscle and the superficial border of the femur. The VL muscle thickness was measured at a point 10% lateral to the circumference of the thigh from the RF and VI measurement point. The VM is measured at a point 12.5% medial to the circumference of the thigh form 20% of the distance between ASIS and superior pole at the patella. To measure VMO, the transducer is placed 4 cm above and 3 cm medially from the superior border of the patella. The VL, VM, and VMO muscles thickness were defined as the distance between the superficial border and deep border of the muscle. The depth and gain of the image were adjusted to show the femur and muscle boundaries in the center of the screen. The thickness of each muscle was analyzed through ImageJ software (National Institutes of health, Bethes-da, MD, USA), which was derived as the average value of three equally
spaced lines on the muscle belly. Each muscle was recorded three times for image analysis after measurement. The order of measurement was the unaffected limb, then the affected limb. The quadriceps muscle thickness measurement utilizing the portable ultrasound had excellent inter-rater reliability (Intraclass Correlation Coefficients (ICCs) 0.95-0.97) and acceptably good inter-rater (ICCs 0.62-0.90) [25,26].
5 Isokinetic knee extension strength test
A Humac NORM isokinetic dynamometer (Cybex, Computer Sports Medicine Inc, Stoughton, MA) was used to measure isokinetic muscle strength during knee extension. Concentric isokinetic knee extension strength was measured at low velocity (60°/sec) to examine the extent of muscle recovery after ACLR [27]. The dynamometer was calibrated before the start of the study according to the operating manual. The range of motion from extension (0°) to flexion (90°) was set. The test was conducted while the subject was seated in a chair with a backrest of 85 de-grees. After moving the chair to an appropriate distance from the dynamometer, align the dynamometer axis of rotation and the knee axis of rotation in a straight line. During the test, the stabilizing straps were used on the participant’ s torso, waist, and thigh to prevent irrelevant movement of the body. The test was performed first on the contralateral limb and then on the ACLR limb. The examiner instructed the subject to perform as quickly and powerfully as possible. All participants performed the 5 repetitions with maximum effort after 4 times for practices followed by 1-minute rest [23]. The other side was performed in the same method. The peak torque according to the velocity was recorded, which was expressed as Newton metre (Nm). The software (HUMAC 2009, v.9.7.1) was used to process the recorded data. Average peak torque of the three trials was divided by the participant’ s weight for normalization. The normalized peak torque value was used for data analysis. The isokinetic strength test using a dynamometer showed good to excellent reliability with ICCs values ranging from 0.74 to 0.86 [28].
6 Limb symmetry index (LSI)
The LSI is an index used as an objective criterion for returning to sports by comparing functions between the injured limb and the unin-jured limb [15,18]. The LSI is primarily used to measure quadriceps strength and hop tests after ACLR and is used as an indicator of return to sport [29]. The LSI for muscle thickness and isokinetic knee extension strength was calculated by dividing the involved limb by the uninvolved limb and multiplying by 100. Values of the LSI were expressed as a percentage (%) [29].
7 Statistical analysis
This study used the Jamovi 2.2.1 software (Jamovi Project, Sydney, Australia) for statistical analysis. In this study, a non-parametric test was conducted because the sample size was too small. The Mann Whitney-U test was used to compare muscle thickness, isokinetic knee extension strength for the reconstructed limb between the two groups, as well as the LSI. The Rank-biserial correlation (r) was used to calculate the effect size of the non-parametric test, and the effect size was interpreted as 0.1 is small, 0.3 is medium, and 0.5 is large [30]. The statistical significance level of α was set to .05 for analysis.
RESULTS
1 Comparison of reconstructed limbs between two groups
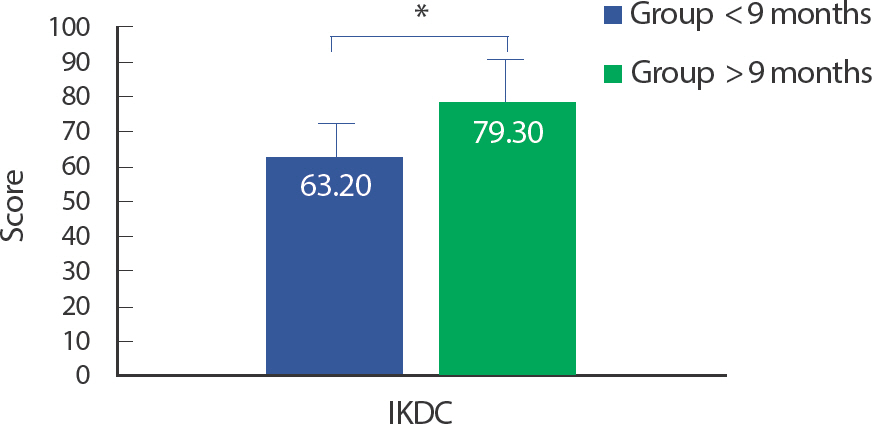
1) IKDC
The IKDC score for the reconstructed limb of the two groups was presented to Table 2 and Fig. 2 The group >9 months (63.20, 57.75-67.27) showed much higher IKDC scores compared to the group <9 months (79.30, 68.67-86.83). There was a significant difference between the two groups in the IKDC score for the reconstructed limb (Z= 12.00, p =.012).
Fig. 2
Fig. 2IKDC Score for reconstructed limb between two groups. Asterisk indicates statistically significant differences (p< .01).
2) Muscle thickness
The muscle thickness for the reconstructed limb of the two groups was presented to Table 3 and Fig. 3 The VM for the reconstructed limbs was found to be significantly larger in the group >9 months (28.59, 27.32-30.90) compared to the group <9 months (23.64, 20.17-26.43), and a significant difference was found between the two groups (Z=12.00, p =.014). Conversely, no significant difference was found between the two groups in the thickness of other muscles. In this regard, there was no significant difference in the RF of the reconstructed limb between the two groups (Z=33.00, p =.573), and the VI and VL of the reconstructed limb also did not show a significant difference between the two groups (Z=19.00, p =.068, both). Similarly, VMO also did not show a significant difference between the two groups (Z=19.00, p =.068).
3) Isokinetic knee extension strength
The normalized knee extension peak torque for the reconstructed limb of the two groups was presented to Table 4 and Fig. 4 The group >9 months (2.89, 2.55-3.46) also showed higher normalized knee extension peak torque for reconstructed limb than the group <9 months (1.97, 1.82-2.31), which was a statistically significant difference in the normalized peak torque (Z=16.00, p =.034).
Fig. 3
Fig. 3Muscle thickness for reconstructed limb between two groups. Asterisk indicates statistically significant difference (p<.05).
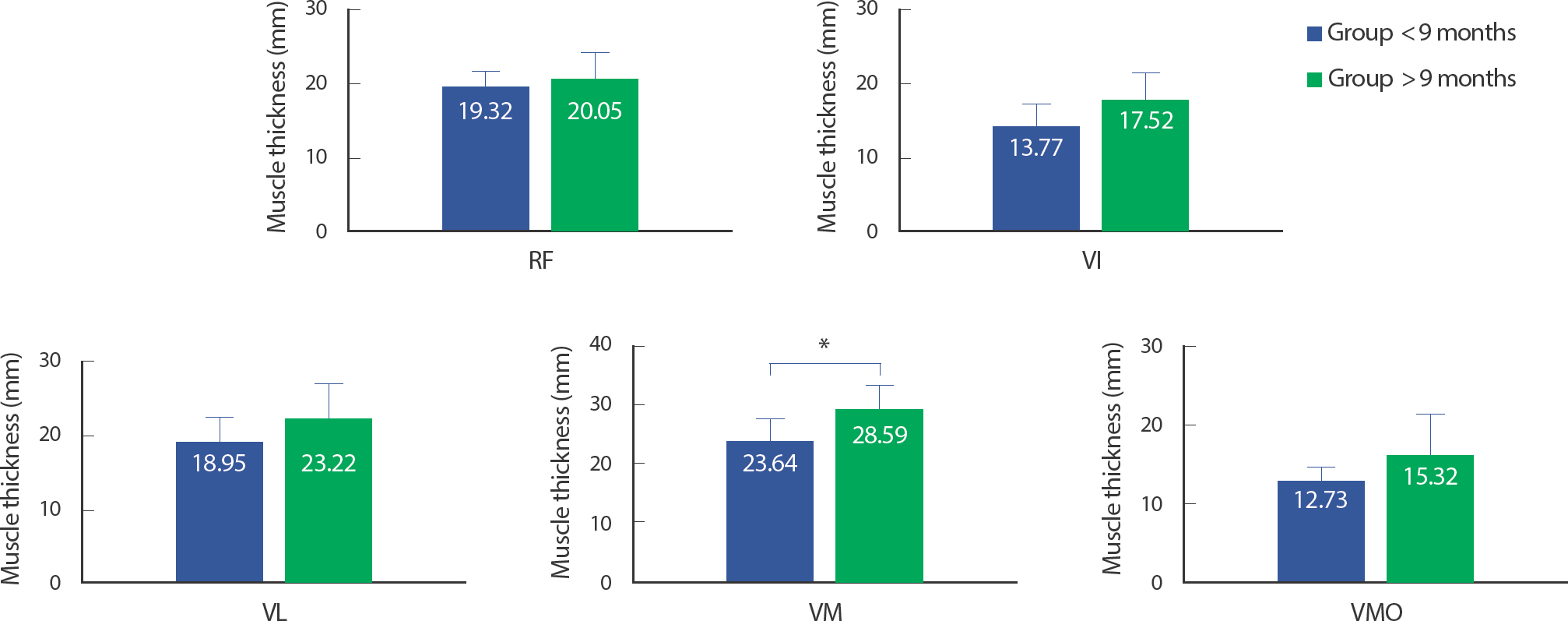
Fig. 4
Fig. 4Isokinetic knee extension strength for reconstructed limb between two groups. Asterisk indicates statistically significant difference (p<.05).
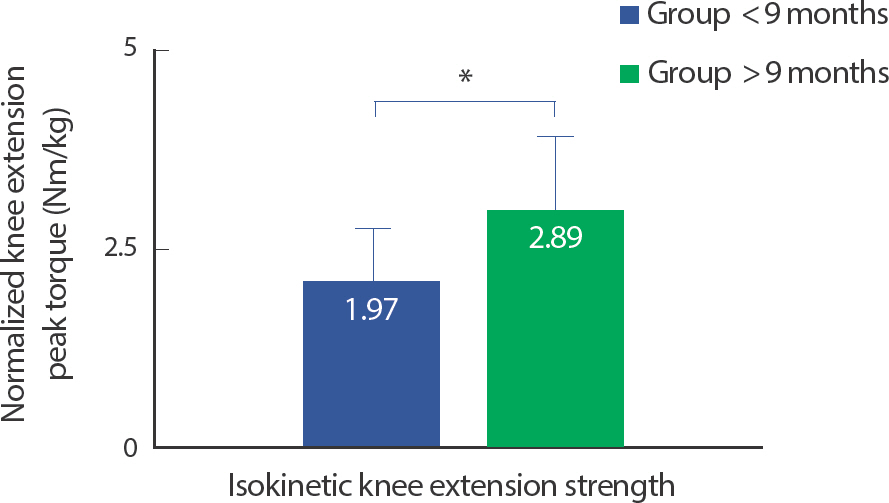
Table 3
Muscle thickness for reconstructed limb between two groups (Median, IQR)
2 Comparison of LSI between the two group
1) Muscle thickness
The LSI for muscle thickness between the two groups was presented to Table 5 and Fig. 5. The LSI of VM showed significant differences between the two groups (Z=10.00, p =.006). The LSI of VM in the group >9 months (90.87, 87.05-95.53) was significantly higher than that in the group <9 months (79.41, 72.77-80.16). Also, the LSI of VI in the group >9 months (95.40, 89.46-97.58) was higher than that in the group <9 months (77.19, 57.34-87.33), and a statistically significant difference was found (Z=10.00, p =.006). However, the LSI of VL did not show a statistically significant difference between the two groups (Z=20.00, p =.083).
Likewise, there were no statistically significant differences in the LSI of RF and VMO between the two groups (RF: Z=37.00, p =.829; VMO: Z=20.00, p =.083).
2) Isokinetic knee extension strength
The Table 6 and Fig. 6 showed that LSI for normalized knee extension peak torque. Unlike normalized knee extension peak torque for reconstructed limb, there was no significant difference in the LSI for normalized knee extension peak torque between the two groups (Z=25.00, p = .375).
Fig. 5
Fig. 5LSI of muscle thickness between two groups. Asterisk indicates statistically significant difference (p< .01).
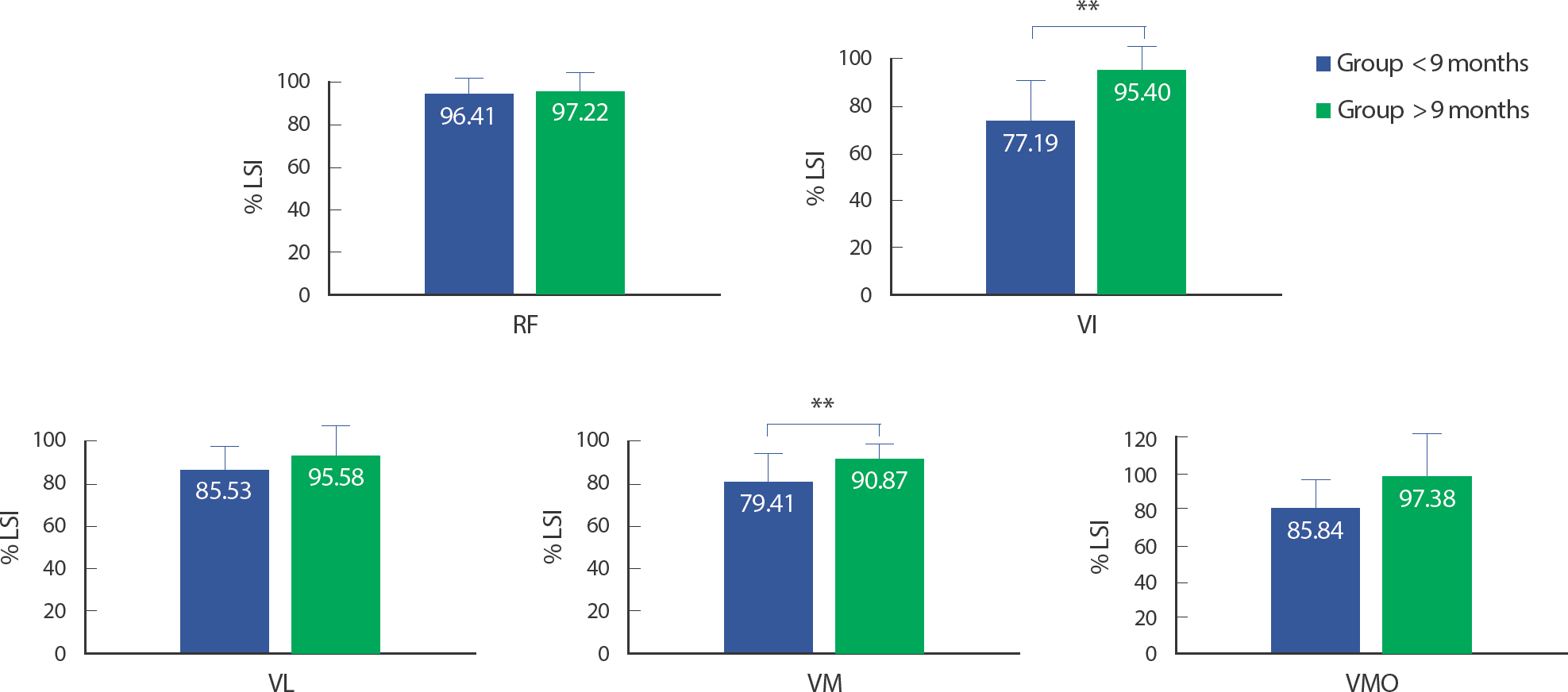
Fig. 6
Fig. 6LSI of isokinetic knee extension strength between two groups. tween two groups. Asterisk indicates statistically significant difference (p<.05).

Table 5
LSI of muscle thickness for reconstructed limb between two groups (Median, IQR)
DISCUSSION
The purpose of this study was to evaluate muscle size and function based on 9 months after ACLR. Significant differences were found between the two groups in IKDC, VM thickness, isokinetic knee extension strength for the reconstructed limb. In addition, the LSI for VI and VM were significantly higher in the group >9 months after ACLR compared to the group <9 months.
Several studies have reported that quadriceps muscle atrophy was prominently observed in patients who underwent ACL reconstruction [2,3,5]. The quadriceps muscle is mainly responsible for knee extension, and each muscle had a different function, so it is important to identify the atrophied muscle among the quadriceps muscles. The main result of this study was that the VM thickness was significantly thicker in the group >9 months than in the group <9 months, and it was consistent with previously reported studies. There is research that investigated the VM thickness of patients who underwent ACLR immediately after surgery and 7 days after surgery. As a result, VM thickness was significantly decreased immediately and 7 days after surgery compared to before surgery [31]. In addition, the VM volume of patients who returned to the preinjury activity level 1 to 2 years after ACLR was still reduced compared to the healthy limb [32].
While the VI did not show a significant difference between the two groups, the large effect size (r=0.525) was found. A previous study reported a significant decrease in VI thickness of the reconstructed limb 2–3 days after ACLR and the muscle thickness reduction was continued until 7 days after surgery [3]. The current investigation could support the previous findings and it may influence to another functional task such as isokinetic knee extension. From a physiological point of view, muscle atrophy appears to have occurred due to an imbalance between muscle synthesis and breakdown. In other words, muscle mass is maintained through an appropriate balance between muscle synthesis and muscle breakdown rates, and most muscle atrophy is caused by decreased muscle protein synthesis and increased muscle protein breakdown [33]. Weakened muscle protein synthesis in the state of muscle disuse is reported as the main cause of muscle mass loss [34]. In particular, the quadriceps muscle is more vulnerable to fiber type transition than muscles dominated by fast-twitch fibers during muscle disuse [33]. As such, the ACLR has been found to cause muscle atrophy in both the short and long term. Therefore, the importance of rehabilitation focusing on each muscle of the quadriceps muscle is raised in the early stage after ACLR.
In this study, the group >9 months after ACLR showed significantly greater normalized knee extension peak torque compared to the group <9 months. Quadriceps muscle strength is considered an important factor for successful return to play after ACLR [35]. A previous study showed that there was a significant correlation between a decrease in CSA and a decrease in knee extensor muscle strength as a result of a patient’ s MRI scan 7 months after ACLR [2]. Therefore, the restoration of the muscle thickness would be critical for muscle function assessment. Although the difference in VI thickness of the reconstructed limb between the two groups was not statistically significant in the present study, it was reported that the effect size was large. The VI muscle is an important muscle for knee function and locomotion, and it is closely related to functional performance such as knee extensor torque and explo-sive movement [36]. In a study of people with an average ACLR of 33 months, it was revealed that the CSA of the VI had a strong correlation in predicting knee extension MVIC, and the CSA of the VM had a moderate correlation. Also, combining the CSA of VM and VI also had a strong correlation in predicting knee extension MVIC. As such, the CSA of VM and VI is thought to be an important factor in knee extensor strength after ACLR [4]. Further, a positive correlation was found between VI muscle thickness and knee extension force in healthy individuals, which was considered to be a better predictor of knee extension force [36]. These results support the results of this study, and it seems that the decrease in muscle morphology after ACLR influenced the decrease in knee extensor muscle strength. For this reason, it can be suggested that emphasis should be focused on VM and VI recovery in the early stages after ACLR.
Significant differences were found in VM and VI in LSI between groups >9 months and groups <9 months, and the effect sizes were large (r=0.75, both). Several studies have reported an RTP acceptance criterion of 85-90% of LSI in functional testing such as hop tests and isokinetic strength test [18]. It is emphasized that bilateral limb comparison is necessary to confirm the recovery of knee function after ACLR. The LSI is a commonly used index for comparing the affected side to the healthy side, and is associated with better RTP rate and lower reinjury rates [29]. Although management of both the involved and uninvolved limb for RTP is important during rehabilitation after a unilateral injury,
traditional rehabilitation programs concentrate on the functional recovery of involved limb only [37]. Previous research has reported that surgery of the involved limb may deteriorate the function of the uninvolved limb during rehabilitation [38]. As such, the LSI results of the current study can support previous study that it is important to manage not only the involved limb but also the uninvolved limb during the postoperative rehabilitation period.
A large difference in knee function between the bilateral limb leads to secondary injuries in the future, which ultimately exacerbates the quality of life [39,40]. That is, it is important to manage it early after ACLR in order to minimize the difference in function of the bilateral limbs. A systematic review reports that early rehabilitation after ACLR has positive effects on strength, functional performance, and RTP [41]. So, the importance of rehabilitation focusing on each muscle of the quadriceps muscle is raised in the early stage after ACLR.
Limitations The current study had some limitations. First, the sample size in this study was too small, and the sex ratio between each group was not consistent. Since there may be differences in muscle characteristics or strength depending on gender, it is necessary to match the sex ratio between groups in future studies. Second, the surgeons of the subjects who participated in this study were not the same. Even in the same operation, each surgeon may have different surgical methods and procedures, so it is necessary to consider this in future studies. Third, the rehabilitation period after surgery for the participants in this study was not set. Since the rehabilitation period may affect the results of this study, it is suggested that the rehabilitation period should also be controlled in the future.
CONCLUSIONS
This study compared quadriceps muscle thickness and isokinetic knee extension strength at 9 months after ACLR. The VM thickness and isokinetic knee extension strength of the reconstructed limb showed a significant increase in the group >9 months compared to the group <9 month. And the LSI for VM and VI thickness was significantly greater in the group >9 months than group <9 months. The current investigations could suggest that early rehabilitation focusing on specific muscles of the quadriceps is necessary after ACLR. Therefore, further research on rehabilitation methods to improve atrophy and weakness of specific muscles after ACLR is required.